In today’s world, sexual health awareness is crucial for maintaining overall well-being. Gonorrhoea, a common sexually transmitted infection (STI), can be transmitted through various forms of sexual contact, including oral sex. Understanding the risks associated with gonorrhoea from oral exposure, as well as the importance of testing, is vital for proactive sexual health management. This article will delve into the risks of gonorrhoea, the testing process, and how to protect oneself and partners from infection.
Understanding the Risks: Gonorrhoea from Oral Sex Exposure
Gonorrhoea is primarily caused by the bacterium Neisseria gonorrhoeae and is often transmitted through unprotected sexual contact. While many people are aware of the risks associated with vaginal or anal sex, oral sex is frequently overlooked. The infection can manifest in the throat, leading to a condition known as pharyngeal gonorrhoea. Symptoms may be mild or absent, making it easy to unknowingly transmit the disease to partners.
The likelihood of contracting gonorrhoea through oral sex is often influenced by several factors, including the presence of cuts or sores in the mouth or throat, the sexual practices involved, and whether either partner is infected. Understanding these risks is essential. Regular testing and open communication with partners can help mitigate the potential spread of the infection and protect overall sexual health.
It’s also important to note that gonorrhoea can often co-occur with other STIs, such as chlamydia and syphilis. This makes it crucial to get comprehensive testing if you believe you’ve been exposed. Staying informed about these risks empowers individuals to make safer choices and encourages responsible sexual behavior.
A Guide to Testing: How and When to Check for Gonorrhoea
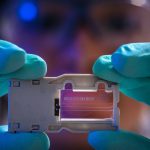
Testing for gonorrhoea typically involves a simple procedure. For oral exposure, healthcare providers may perform a throat swab to check for the presence of the bacterium. This process is quick, usually painless, and can be conducted in a variety of healthcare settings, including clinics, hospitals, or dedicated sexual health centers. It’s important to consult a healthcare professional who can provide guidance on the best testing methods based on individual risk factors.
Timing is also a crucial aspect of testing. Experts recommend getting tested approximately one to two weeks after potential exposure to ensure accurate results. However, if any symptoms arise—such as a sore throat, difficulty swallowing, or unusual discharge—it’s advisable to seek testing immediately. Regular screening is especially important for sexually active individuals, as it helps catch infections early, reducing the risk of complications and further transmission.
Interpreting test results can be anxiety-inducing, but it’s essential to approach them with a clear mindset. A positive result indicates an infection that can be treated with antibiotics, while a negative result suggests that no infection is present at that time. Regardless of the outcome, maintaining open communication with healthcare providers and partners is crucial for ongoing sexual health management.
Understanding the risks associated with gonorrhoea from oral sex exposure and knowing how and when to get tested can significantly empower individuals in their sexual health journey. By prioritizing regular testing, open communication, and safe practices, we can collectively work towards reducing the incidence of STIs like gonorrhoea. Remember, seeking help and guidance is not just a matter of personal health—it’s a step towards fostering a more informed and responsible community. Take charge of your sexual health and encourage those around you to do the same.