===
Gonorrhoea is a prevalent sexually transmitted infection (STI) that can have serious health implications if left untreated. Understanding the testing and treatment timelines is crucial for maintaining sexual health. This article aims to provide clear guidance on what to expect during gonorrhoea testing, when to get tested, and the effective treatment options available. By equipping individuals with the knowledge they need, we can foster a more informed and healthier community.
Understanding Gonorrhoea Testing: What to Expect and When
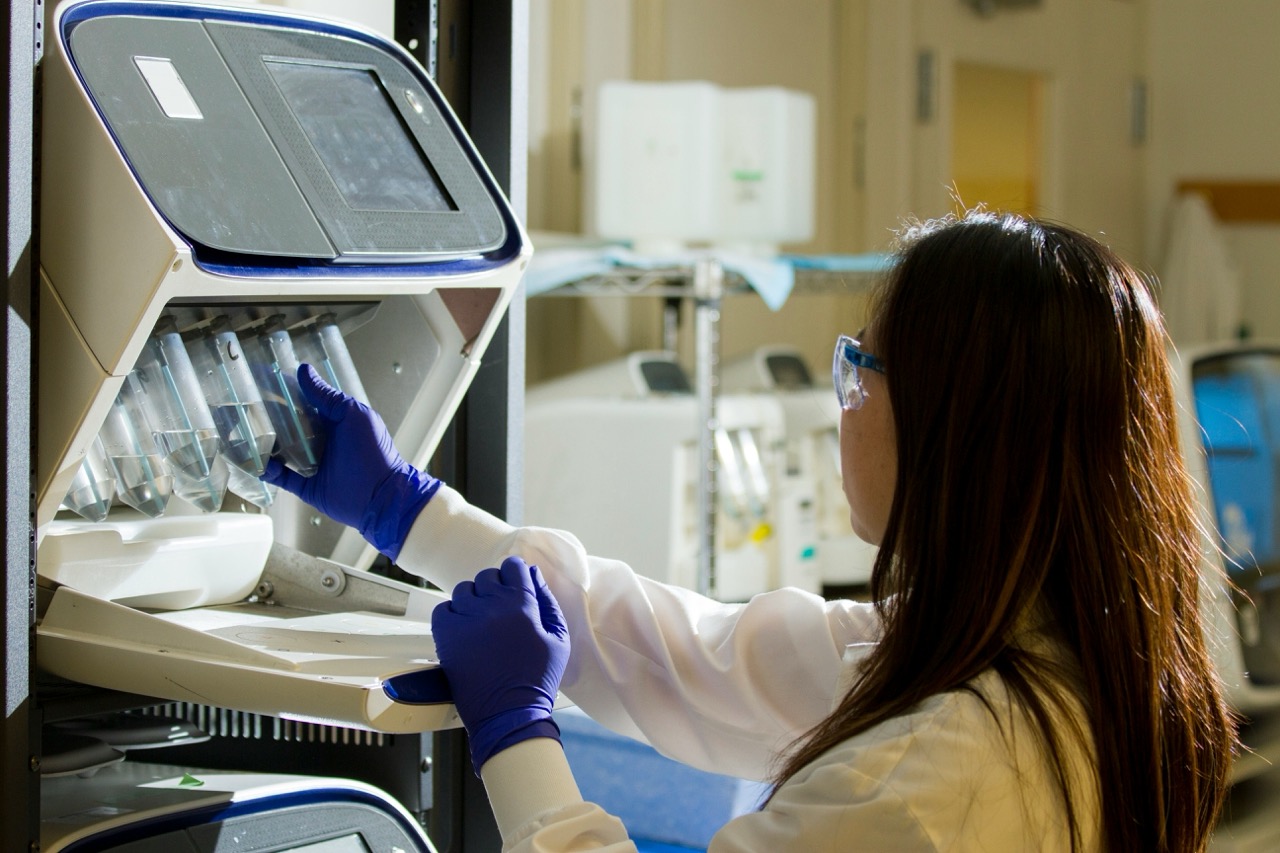
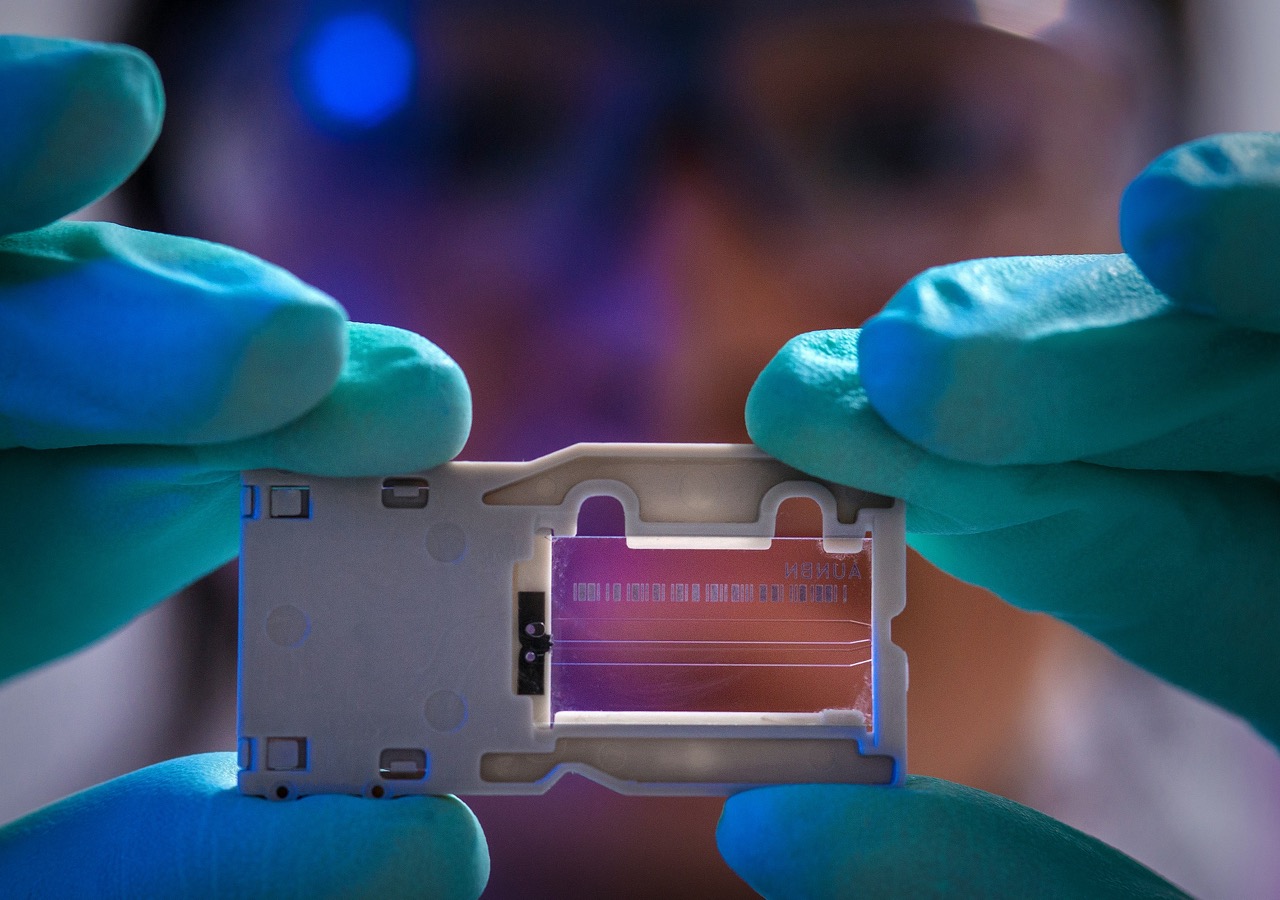
Gonorrhoea testing is a straightforward process that often involves a urine test or a swab from the affected area, such as the throat, rectum, or cervix. Generally, individuals should consider getting tested if they have recently had unprotected sex, experience symptoms like unusual discharge, pain during urination, or swelling in the genital area. The Centers for Disease Control and Prevention (CDC) recommends regular testing for sexually active individuals, especially those with multiple partners or those who engage in high-risk behaviors. Testing is often quick, taking only a few minutes, and can be done at many clinics and healthcare facilities.
After a test, results typically take anywhere from a few hours to a week, depending on the type of test administered and the laboratory used. Most clinics will contact patients directly to inform them of their results, and it’s essential to follow up with healthcare providers if there are any delays or concerns. Understanding your results is crucial; a positive test for gonorrhoea means that treatment is necessary, while a negative result indicates no infection, although it’s still wise to continue regular testing if risk factors are present.
It’s also important to note that testing for gonorrhoea can be done alongside screening for other STIs, such as chlamydia and syphilis. This is particularly beneficial as many STIs can occur together. Regular screenings and open communication with partners about sexual health can significantly reduce the risk of transmission and complications associated with gonorrhoea.
Effective Treatment for Gonorrhoea: Timelines and Options
When gonorrhoea is diagnosed, timely treatment is essential for both individual health and preventing further transmission. The standard treatment for gonorrhoea typically involves a dual therapy approach, which includes an injection of ceftriaxone and oral azithromycin. This combination is effective against the strains of gonorrhoea currently circulating. Treatment is usually administered in a healthcare setting, ensuring that patients receive proper guidance and support while being treated.
Following treatment, patients are generally advised to abstain from sexual activity for at least seven days or until they have completed treatment and had a follow-up test, if recommended. It’s also essential for sexual partners to be notified and tested, as reinfection can occur if they are not treated simultaneously. Healthcare providers may recommend retesting for gonorrhoea approximately three months after treatment to ensure that the infection has been completely cleared.
In the case of persistent or complicated gonorrhoea infections, additional treatment strategies may be necessary. Some patients may require hospitalization or more aggressive antibiotic regimens, especially if complications such as pelvic inflammatory disease occur. Open communication with healthcare providers about any ongoing symptoms or concerns is vital for effective management and recovery.
===
Understanding the timelines and procedures associated with gonorrhoea testing and treatment empowers individuals to take charge of their sexual health. Regular testing and prompt treatment not only promote personal well-being but also contribute to the overall health of the community. By fostering an environment of knowledge and compassion, we can reduce the stigma surrounding STIs and encourage proactive health measures. Remember, prioritizing your sexual health is a vital step towards a healthier future.