Chlamydia is one of the most common sexually transmitted infections (STIs) worldwide, often affecting young adults and those with multiple sexual partners. Understanding the nuances of testing for chlamydia, particularly the timing of tests, is crucial for effective management and treatment. This article explores the implications of testing for chlamydia too late, the importance of timely testing, and what steps to take if you find yourself in this situation.
Understanding Chlamydia: Symptoms and Risks Explained
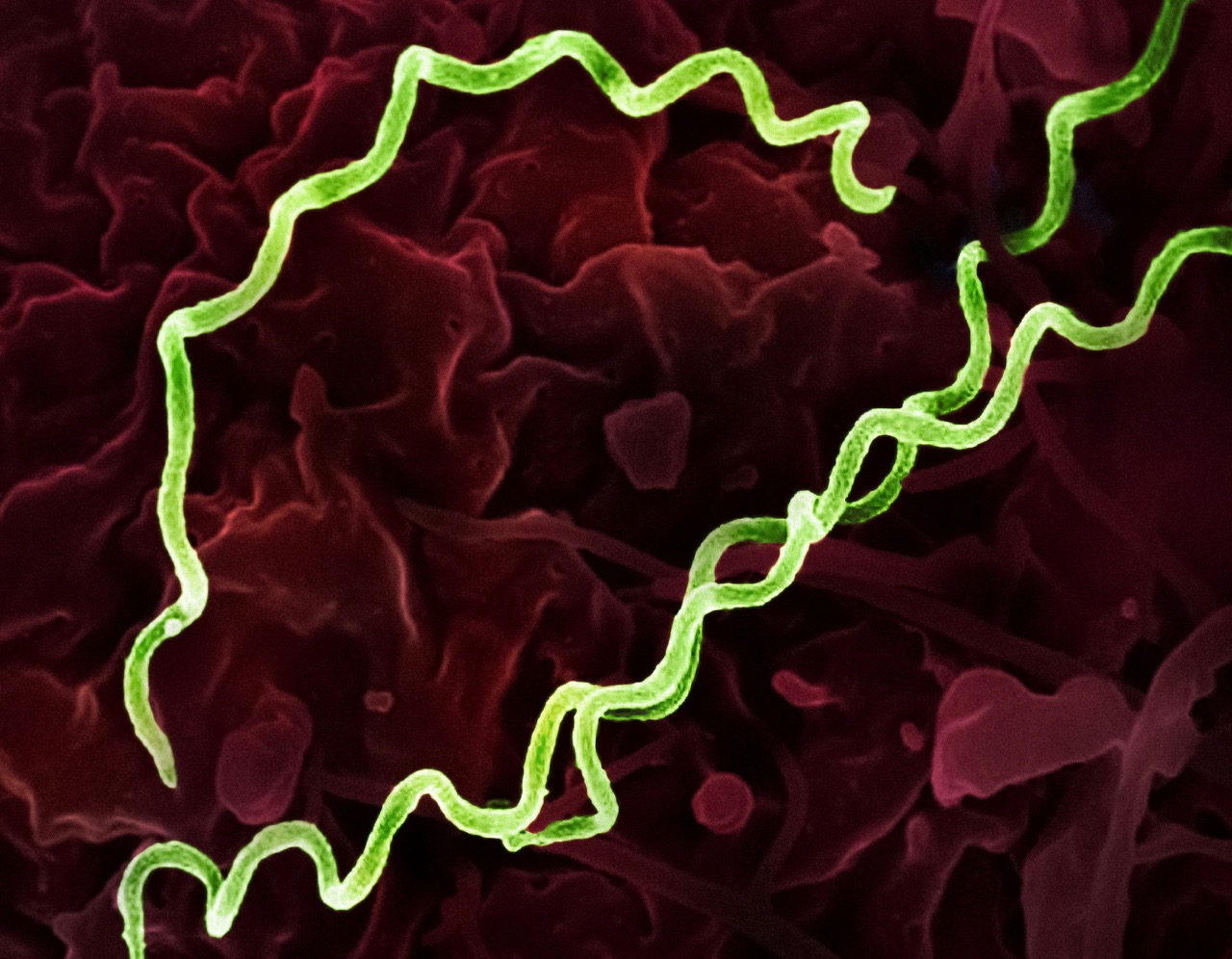
Chlamydia is caused by the bacterium Chlamydia trachomatis and is primarily transmitted through sexual contact. Many individuals do not exhibit symptoms, making it easy to overlook the infection. When symptoms do present, they can include abnormal discharge, painful urination, and pelvic pain in women, and discharge or pain during urination in men. Recognizing these symptoms is crucial, but many people may not connect their experiences to an STI, which puts them at higher risk for complications.
Untreated chlamydia can lead to severe health issues, including pelvic inflammatory disease (PID), infertility, and increased susceptibility to other STIs, including HIV. Moreover, the infection can spread to partners, perpetuating a cycle of transmission. Because of its asymptomatic nature, awareness and education about chlamydia are vital, emphasizing the importance of regular testing, particularly for sexually active individuals and those at higher risk.
Given its potential complications, understanding the risks associated with chlamydia is essential. The infection often goes unnoticed until it has progressed, making it critical for sexually active individuals to remain vigilant about their sexual health and seek testing if they suspect exposure or if they are experiencing symptoms.
Timing Matters: When to Get Tested for Chlamydia
The Centers for Disease Control and Prevention (CDC) recommends that sexually active women under 25, as well as older women with new or multiple sex partners, get tested for chlamydia annually. For men who have sex with men, regular testing is also advised. Testing should occur after any new sexual partner or after unprotected sex, even if no symptoms are present. The key is to prioritize your sexual health through proactive testing.
Testing for chlamydia is most effective when done after a potential exposure period. Typically, health professionals suggest waiting about 7 to 14 days after potential exposure before getting tested. This timeframe allows for accurate detection of the bacteria, as testing too early can result in false negatives due to the bacteria not being present in detectable levels yet.
It’s important to remember that even if you feel fine, you may still carry the infection. Regular testing is an essential part of responsible sexual health, and it helps not only protect yourself but also your partners. Making testing a routine part of your health care can significantly reduce the risk of complications associated with untreated chlamydia.
Late Testing: What Happens If You Miss the Window?
Testing for chlamydia too late can lead to various complications. If a person has been infected and does not seek testing until symptoms appear or after a significant delay, they may face serious health issues. For women, late diagnosis can result in PID, while men might experience epididymitis, which is inflammation of the tube at the back of the testicle. Both conditions can have lasting effects on reproductive health.
Additionally, being tested late increases the likelihood of transmitting the infection to partners. This not only affects their health but can also contribute to the ongoing cycle of chlamydia in the community. The longer the infection goes untreated, the more difficult it can become to manage, and the more potential for complications increases.
If you suspect that you may have delayed testing, it’s crucial to seek medical attention promptly. Health care providers can provide guidance on the next steps, including appropriate testing and treatment options. The sooner you address the issue, the better your chances for effective treatment and recovery.
Next Steps: Interpreting Results and Seeking Treatment
Understanding your test results is vital. If you test positive for chlamydia, don’t panic; it is a common infection and highly treatable. Most healthcare providers will prescribe antibiotics to clear the infection, and it’s essential to complete the full course of medication, even if symptoms resolve quickly. Your sexual partners should also be informed and tested to prevent reinfection and further spread of the disease.
If your test results are negative but you still experience symptoms, follow up with your healthcare provider. It’s possible to have a different infection or another issue that requires attention. Open communication with your healthcare provider can provide clarity and reassurance, allowing you to manage your sexual health actively.
Finally, consider discussing preventive measures with your healthcare provider. Regular testing, consistent use of condoms, and limiting the number of sexual partners are effective strategies to reduce your risk of STIs, including chlamydia. Empowering yourself through education and proactive health measures is a key component of maintaining sexual wellness.
Chlamydia testing is a critical aspect of sexual health that should not be overlooked. By understanding the timing and implications of testing, individuals can take charge of their sexual health and seek timely treatment when necessary. It’s never too late to prioritize your well-being; if you have concerns or suspect exposure, do not hesitate to reach out for help. Remember, open communication with healthcare providers, regular testing, and education are your best tools for navigating sexual health effectively.